NAACOS Fall 2019 Conference – A Focus on Care Coordination and Finding Value
At the end of September, Verinovum traveled to Washington, DC, to attend the National Association of ACOs (NAACOS) Fall 2019 Conference, an event that NAACOS promised would “provide the road map for ACOs navigating this high-speed, healthcare freeway into the future.”
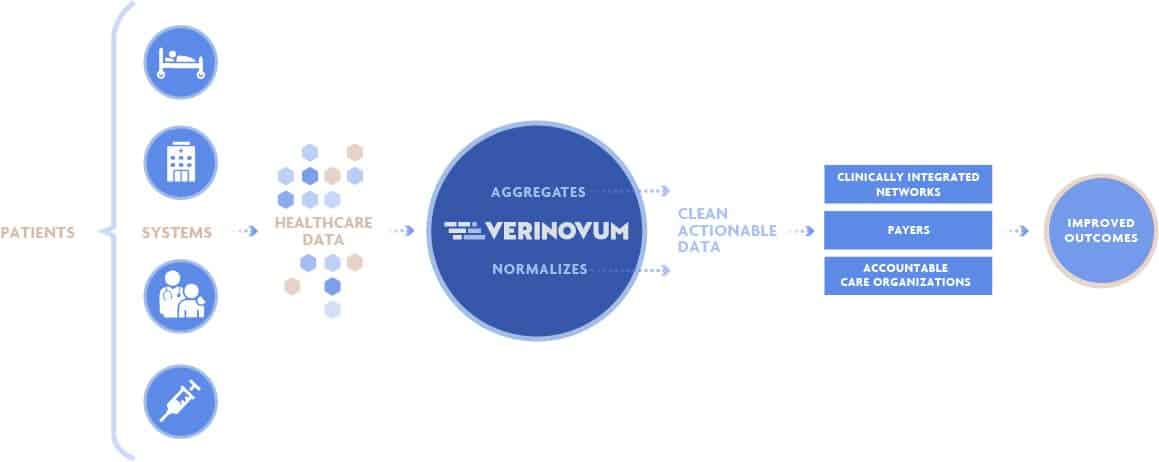
As the conference website noted, “ACOs are positioned at the intersection of value-based payments, population health, care coordination, innovation, transformation, and collaborations among Medicare, Medicaid and commercial payers.” Verinovum understands these issues, as well as the necessity for clean, enriched data to help hospitals and ACOs meet these challenges head-on, so we headed to the event to hear what was on the collective minds of the industry leaders.
The common thread throughout all the topics discussed was the desire to close the loop on coordinated care and to find true value (a balance between cost and quality), all with the goal of improving patient outcomes.
1. Social Determinants of Health
Because factors such as a patient’s social, emotional, environmental and financial situation can have a major impact on chronic disease, emergency department visits, and hospital readmissions, learning how to care for patients and overcome any social determinants of health (SDOH) barriers has recently become of great interest to healthcare stakeholders, and was one of the hot topics at the NAACOS conference.
A presentation from the Physician Organization of Michigan ACO, “Addressing the Needs of Community Health through Organizational Responsibility,” effectively summarized SDOH challenges and sharing what they are doing to improve health in their community.
For example, the Physician Organization of Michigan ACO has created a committee to increase communication and understanding between patients and providers. Committee members in their ACO Medicare Beneficiary Advisory Committee are all Medicare beneficiaries, not advocacy organizations or other entities. They are of diverse demographic, professional, and educational backgrounds across Michigan, and are nominated to the committee by providers.
The committee has done a great deal of positive work to impact SDOH, including developing patient-facing materials for annual wellness visits, providing input on efforts towards decreasing social isolation among aging adults, and offering feedback on various patient experiences.
What Creates Health?
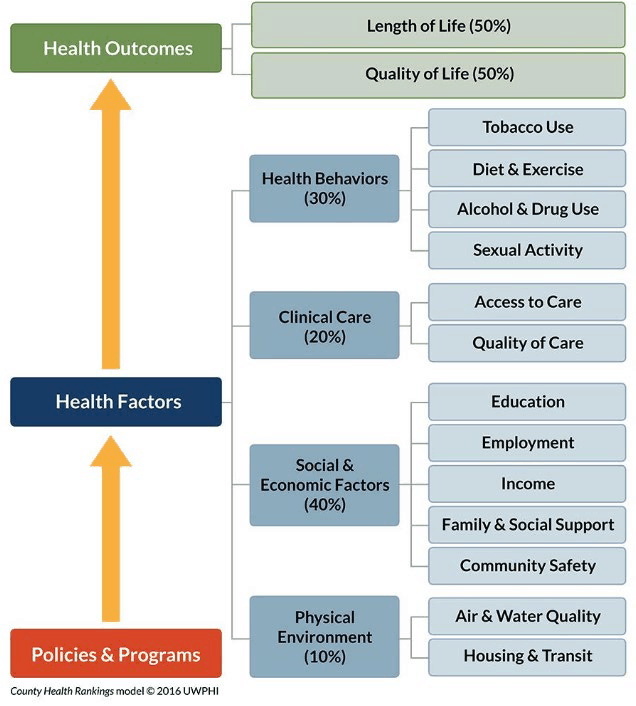
*from the Physician Organization of Michigan ACO, “Addressing the Needs of Community Health through Organizational Responsibility” presentation, NAACOS Fall 2019 conference
2. Embracing Digital Patient Care
One theme we heard a great deal about at the conference was the shift to digital and virtual care. Similar to addressing social determinants of health, organizations are realizing they can improve care coordination and thereby patient outcomes by extending patient interactions beyond the four walls of the hospital.
Unsurprisingly, technology and digital options are emerging as effective ways to impact patient health. One presentation, “New Models for Success at the Intersection of Innovation & Value-Based Care” from LifeBridge Health (an integrated delivery network in Baltimore), gave a comprehensive overview of the current, unsustainable costs of healthcare and illustrated some ways that virtual care and other technology advancements can help rein those costs in.
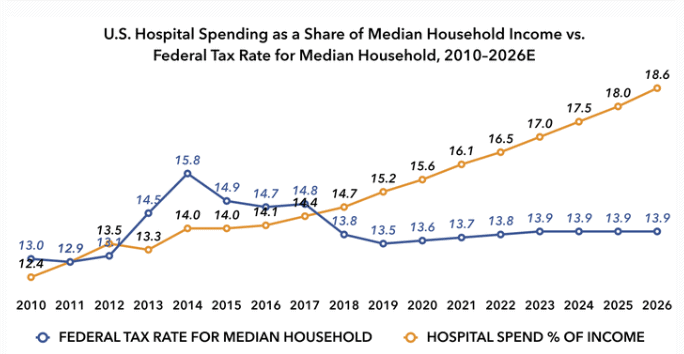
*from the LifeBridge Health, “New Models for Success at the Intersection of Innovation & Value-Based Care” presentation, NAACOS Fall 2019 conference
For example, LifeBridge offers telehealth consultations, an automated patient engagement app, digital check-in kiosks, online scheduling, and more. Depending on the department or service in which a hospital applies virtual and digital solutions, positive results could include:
- More seamless care coordination, with reduced potential for human error
- Increased efficiency through automation of manual processes
- Enhanced patient participation and awareness in their health journey
- Providing patients with real-time access to the medical team
- Increased capacity/productivity of specialists and other clinicians
LifeBridge has seen some positive results by implementing methods like these. For example, those patients who participated in the IDN’s interactive patient engagement program (which includes daily push notifications, continuous assessments, secure messaging, remote monitoring, reminders, etc.) had a 15% lower 30-day ED revisit rate, and a 16% (Northwest) and 31% (Sinai) lower 30-day inpatient revisit rate than patients who did not participate.
3. Alternative Sites of Care
In addition to using telehealth and other digital care techniques, another way to cope with rising healthcare costs and stretched physician capacity is to move care from hospitals into other settings when possible. This was the topic of the Atlantic Health System presentation, “Benefit Designs for Alternative Sites of Care.”
As the presentation noted, hospital admissions make up a third of all U.S. health spending, yet at least 10% of hospital admissions do not require the full array of inpatient services, such as in-house specialists or operating rooms. As a result, the industry has begun shifting to a variety of outpatient sites, including free-standing emergency departments, health clinics within retail pharmacy chains, skilled nursing facilities, urgent care centers, and Hospital at Home programs.
Atlantic Health System groups the benefits of shifting to such sites into three major categories:
Quality
- More flexibility for both the patient and the caregiver
- Reduced exposure to hospital-acquired conditions: falls and trauma, pressure ulcers, medication errors, infections, etc.
Economic
- Offers additional primary care sites after business hours for improved access to health care services
- Allows more patients to receive certain therapies in the community, such as home IV infusions
- Often far less expensive to payers, purchasers and patients
Satisfaction
- Provides patients more involvement in decision making, positioning them as partners in improving healthcare quality
- Greater convenience; care options closer to where patients live and work
4. Keynote Presentation – Cost and Quality
In addition to these important issues, Will Shrank, MD, Chief Medical and Corporate Affairs Officer of Humana, touched on a few other hot topics during his keynote address, “Which Way Forward?”.
The first of these was the importance of quality measures – more specifically, quality measures that align with the outcomes we all want. He noted that Humana started with more than 1,000 different types of metrics, but that by distilling them through the removal of duplicates and inconsistencies, Humana was able to narrow this down to about 200 meaningful measures, reducing their metrics by 80%.
This is important because when payers are able to identify those metrics which will actually illustrate quality of care, and then work to improve upon those specific values, costs go down while patient outcomes improve.
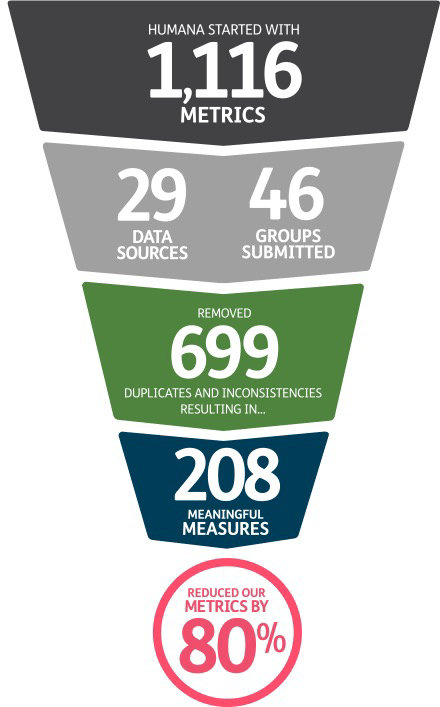
*from the Humana, “Which Way Forward?” presentation, NAACOS Fall 2019 conference
The second issue Shrank covered was pharmacy as the blind spot for physicians when it comes to moving towards truly accountable care. In particular, he said, providers are often unaware of how much patients are paying out of pocket for the drugs they prescribe. Medications – especially specialty drugs – are one of the fastest rising costs in healthcare, Shrank noted, and yet we too often don’t consider drug costs when we talk about value-based care.
How do we Get There?
At Verinovum, we support efforts by ACOs, CINs and payers to move towards value-based care, and we’ve seen that the use cases most healthcare organizations are prioritizing are the very ones covered at this year’s NAACOS event. And while the need for clean, robust, actionable data was an important underlying theme throughout the event, none of the presenters had a solid roadmap for getting there.
A payer or hospital that wants to track social determinants needs complete patient records that show what is happening both within and outside the healthcare facility. An organization looking to move towards virtual and/or digital care methods needs to track readmissions and other outcomes as well as have information about previous tests, current medications, etc. in real-time. Those looking to incorporate non-acute care settings need to ensure that care is coordinated among all parties and that information is not lost somewhere along the patient journey.
In use case after use case, we find that the only way to achieve the results the industry requires is with strong data. Verinovum integrates comprehensive patient records from multiple data sources, cleanses and de-duplicates the information, and continually processes, updates and improves the data in real-time. The result is a comprehensive view of each unique patient record that allows ACOs, CINs and payers to meet the goals most important to them at any given time.
Where will your data take you?